This page is written by leading microsurgical authority, educator and author, Sheldon H.F. Marks, MD, to review some of the key concepts with redo, repeat or “salvage” vasectomy reversal success rates after the first vas reversal attempt failed.
“We wish that we had come here the first time” is what we hear weekly after we perform a redo vasectomy reversal at our full time, vas reversal only center.
Men from every state in the US and more than 85 countries internationally come to see Dr. Marks and Dr. Burrows to have their redo and even redo, redo vasectomy reversals performed after their first attempts elsewhere fails. There are many weeks where the doctors of ICVR perform 2 or 3 redo vas reversals.

“We recently received a photo of a doctor’s two daughters. Several years ago this Maryland physician had a failed first reverse vasectomy locally, then traveled to Chicago for his second unsuccessful vas reversal to a doctor he thought was an expert. That failed and then after doing his research, he and his wife decided that his best chance for a successful repeat vasectomy reversal was here at ICVR. The surgery went great with amazing results, and now he has two beautiful daughters.”
The good news is that our full-time, vas reversal only “Center of Excellence” has a proven, very high redo vasectomy reversal success rates ! In fact, the doctors of ICVR presented our experience with hundreds of redo vasectomy reversals at an international fertility meeting where we showed that the chances for a high success rate at our high volume specialty program is the same here as if the patient never a failed vas reversal before, whether with the same partner or new partner (1)!
Studies have shown that a redo vas reversal is usually still highly successful and even still more cost-effective than moving to in-vitro fertilization (IVF) with ICSI (intra-cytoplasmic sperm injection) (2-4). We just had a patient who had a vas-to-vas connection on both sides elsewhere with a redo vas-to-epididymal bypass here and as of today, just 3 months later, he is already at 20 million motile sperm, totally normal!
We have more than 8000 patients over many decades who travel to ICVR every day. And because each doctor limits his practice to only one reverse vasectomy a day, this means every patient receives the doctor’s full and undivided attention to detail with no pressure to rush to get to subsequent vas reversals that day nor is he fatigued from earlier microsurgeries. Just one a day is the right way to do it.
Why do we have such high success rate with redo vas reversals when others fail?
We assume two opposites when we perform a redo vas reversal to ensure the highest redo vas reversal success rates for each patient. First, that the procedure was performed correctly and that the patient scarred up at the connection from excessive inflammation, which may progress untreated, often from minimal to no follow-up. The other assumption is that the doctor did not do a technically precise multi-layer (3 to 4 layer) closure, which is why the connection scarred and now needs to be redone.
Plus, we found that sometimes the incorrect technique was performed, so that a vas-to-vas connection (VV) may have been performed when the absence of sperm in the vasal fluid indicated that the more challenging vas-to-epididymal bypass (VE) was the correct technique to perform (5). There are many doctors that can’t or won’t perform the epididymal bypass or still use the older, easier one or two layer closures.
Here’s what we do
We treat each patient before, during and after the vas reversal with anti-inflammatory medications to prevent excessive scarring. We also monitor the semen analysis counts frequently after the redo reverse vasectomy, usually every 4 weeks. We stay on top of these results, actively working with each patient closely for many months to be sure that the repair stays open. If there are any concerns with sperm counts or motility, then we are able to intervene during that window of opportunity to get the sperm counts up and to stay up at levels good enough for natural conception! There are some doctors who don’t provide what we believe to be this critical close and extended aftercare.
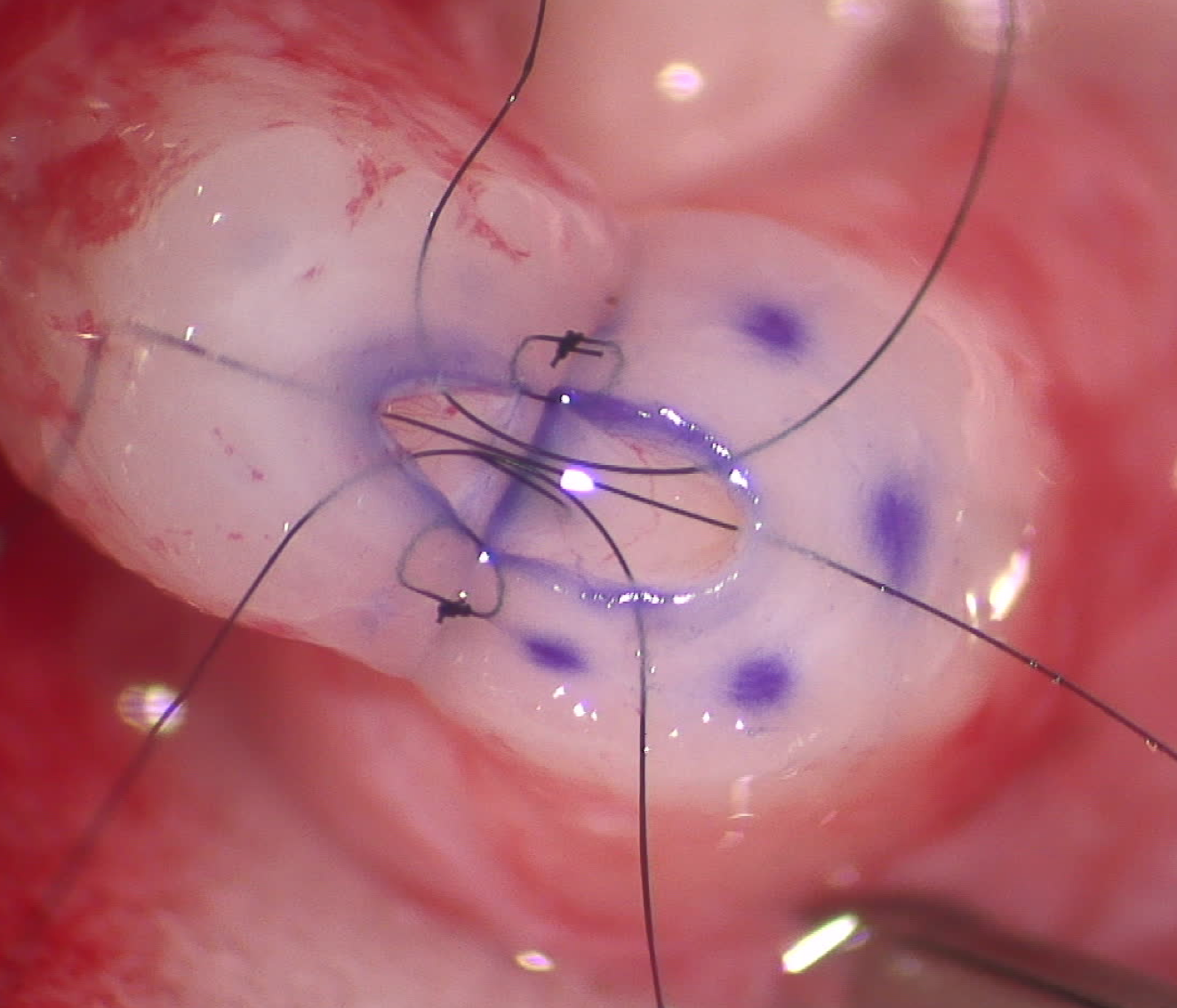 Many patients ask if we do anything technically differently during the redo vas reversal? The truth is we do the exact same microsurgical multi-layer (3 to 4 layer) vasovasostomy, whether this is a first time or if it is a redo redo reverse vasectomy. We have even performed redo redo redo vas reversals with wonderful results and babies. Because we have performed so many thousands of vas reversals, yet just one a day for each doctor, we are able to achieve the highest vasectomy reversal success rate (6).
Many patients ask if we do anything technically differently during the redo vas reversal? The truth is we do the exact same microsurgical multi-layer (3 to 4 layer) vasovasostomy, whether this is a first time or if it is a redo redo reverse vasectomy. We have even performed redo redo redo vas reversals with wonderful results and babies. Because we have performed so many thousands of vas reversals, yet just one a day for each doctor, we are able to achieve the highest vasectomy reversal success rate (6).
Considering what’s at stake, experience matters!
Too often, we can see from the patient’s prior operative note (it is very helpful to have this sent to us) or from findings in surgery that the prior vasectomy reversal doctor performed a vas reversal without checking the vasal fluid for sperm or performing the vas-to-vas connection (VV) when we would have done an epididymal bypass (VE)(7). Some doctor’s may have only “one tool in their toolkit,” the vas-to-vas connection, which may be right for many patients but not for all. We believe in personalized, customized care – doing the right treatment for the right patient at the right time.
Bottom line: What we see at the repeat salvage surgery often involves a tremendous amount of scarring in and around the prior vas reversal connection. There are times when we see retained vasectomy tissues or a sperm granuloma which was left behind, even though we always remove these and teach the importance of removing these at the time of the original vas reversal. We feel that the best results will most often be with a urologist who has completed a formal fellowship after their urology residency, using only high powered surgical microscopes which provide better visualization with far superior vas reversal success rates (8). We have found that we achieve the highest reverse vasectomy success rates when we perform a meticulous multi-layer microsurgical vas reversal using a high-powered surgical microscope which can take about 2 to 2½ hours on average (9).
In order to achieve the very highest vas reversal results and stay up on cutting edge advances, both doctors of ICVR attend yearly specialty fertility society meetings where experts from around the world all get together to talk about how to improve patient and vas reversal care. Because of our desire to provide the highest level of care and improve on our techniques and care, this is an important part of our continuing education. Sadly, many doctors do not attend these meetings. I can only assume that they think that what they learned years ago is still up-to-date.
Of course, redo vas reversals are always more challenging and time consuming with higher risks for complications than with a first time vasectomy reversal. This is another reason to choose wisely the first time, so there won’t need to be second time.
For patients that have had a failed vas reversal or just have questions about a repeat “salvage” reverse vasectomy, contact us to set up a time to talk to either of our 2 microsurgeons – Dr. Sheldon H.F. Marks or Dr. Peter J. Burrows, at no charge, about what we can do to help couples achieve the dream of restoring fertility and having children again. These consults can be in person, by phone or virtually on Zoom, Skype or Face Time most days, evenings and weekends.
This page was reviewed, edited and updated January 8th, 2026, by Sheldon H. F. Marks, MD.
References:
1.Kim SW, Ku JH, Park K, Son H, Paick J-S. A different female partner does not affect the success of second vasectomy reversal. J Androl. 2005;26(1):48–52.
2.Matthews GJ, McGee KE, Goldstein M. Microsurgical reconstruction following failed vasectomy reversal. J Urol. 1997; 157:844-6.
3.Hollingsworth MR, Sandlow JI, Schrepferman CG, Brannigan RE, Kolettis PN. Repeat vasectomy reversal yields high success rates. Fertil Steril. 2007;88(1):217–9.
4.Pasqualotto FF, Agarwal A, Srivastava M, Nelson DR, Thomas AJ. Fertility outcome after repeat vasoepididymostomy. J Urol. 1999;162(5):1626–8).
5.Marks, S.H.F., Perkins A.R., Burrows P.J., Ax R.L., McCauley T.C.. Redo vasectomy reversal intraoperative findings implicate incorrect initial reversal technique in 28% of cases. 64th Ann. Mtng. Amer. Soc. Reprod. Med. Abstract. 2008.
6.Silber SJ, Grotjan HE. Microscopic vasectomy reversal 30 years later: a summary of 4010 cases by the same surgeon. J Androl 2004;25(6):845-859.
7.Kirby EW, Hockenberry M, Lipshultz LI. Vasectomy reversal: decision making and technical innovations. Transl Androl Urol. 2017 Aug; 6(4): 753–760.
8.Fox M. Vasectomy reversal—microsurgery for best results. Br J Urol 1994;73(4):449-53.
9.Schwarzer JU. Vasectomy reversal using a microsurgical three-layer technique: one surgeon’s experience over 18 years with 1300 patients. Int J Androl 2012;35(5):706-13.