This article reviews the treatments for PVPS, prepared by international vasectomy reversal authority Dr. Sheldon Marks, to better understand many of the choices, options and success rates each patient has when considering the care of significant pain after vasectomy.
This is a very brief review of many of the options for PVPS management. It is smart to use this up-to-date information as a foundation for a detailed conversation with doctors about the pros and cons of each option, as well as other treatments that may not be addressed in this summary.
If a man has significant pain after vasectomy that is not resolving on its own over time , then it makes sense to consider these options (1).
Many of these treatments can be done at the same time. It is not a “try one, wait and see if it works and if not, then move to the next” approach. The big question doctors are often asked is when is the right time to move from treatment to treatment and when should more aggressive therapies be considered? in our full time, vas reversal only practice, men always ask when should they have a vasectomy reversal? The answer is that it is totally up to each individual, as there is no absolute right answer for every man. What should be done is what seems right for that person at that time.
We encourage men with significant post-vasectomy pain to use this information as a foundation to create shared decision-making when they talk to the doctors to develop a personalized plan (2). It is not wise nor is it safe to make care decisions based solely on what is written here or what others write on websites or tell people what to do. The good news is that for almost all men, when it seems right, moving ahead with a vas reversal provides high success with dramatic improvement or total relief of the pain in most men (3).
Plus, there are concerns that if one waits too long, with the hope that things will start to get better, then the pain nerve pathways become hardwired so that even with definitive treatment, men may have a much slower recovery with lower chances for successful resolution of the PVPS. Some men want to move to more aggressive treatments and a reverse vasectomy at only 6 to 8 weeks after vasectomy as they are eager to get resolution of the pain while others are still uncertain and want to continue with conservative treatments, even many years after the vasectomy. I had one patient who waited 7 years before he had his vasectomy reversal with excellent results.
Of course, it is totally reasonable to be afraid of a vasectomy reversal surgery for pain when it was a surgery originally that lead to the pain. The difference is that a state-of-the-art multilayer microsurgical vas reversal is the only restorative, reconstructive treatment where many of the other surgical options are destructive.
Men should take into account that as a full time vas reversal doctor, my thoughts below obviously include my own biases based on decades of caring for men with PVPS and my belief that a vasectomy reversal is the best treatment when the time is right.
Here are the most common options for treatment of Post Vasectomy Pain (PVPS) (4)-
Conservative treatments
1. Time– yes, many men will get better over time with no other treatments. Some may even have total resolution of the pain, weeks to months to years after the vasectomy. Others will not. There is no way to know what will happen in the future. A good sign is if things are getting better, though it is normal to expect fluctuations with good and bad days, good and bad weeks.The natural response in a good phase is to back away from a vas reversal, only to regret that and then want to have the surgery when the pain returns.
2. Conservative choices– these can sometimes make one feel better, even if only for a short time, while time run also its course. Cold compresses or heat packs a few times a day, sitting in hot tubs, hot saunas or hot baths, wearing a snug athletic supporter or compression shorts 24/7 for several weeks, avoiding heavy strenuous activity, and reduced sexual activity may help some men. We have found that what works for one may or may not work for another.
3. A new treatment that is gaining popularity is to seek out the care of a physical therapist that specializes in pelvic pain, as this can be very effective for some men. We even have a specialized pelvic pain therapist in our office, but she is only an option for men who live nearby, as the care is a process and not just one visit.
4. Supplements– there are many anti-inflammatory supplements that may help as well. Be careful as they can be very expensive, many are unproven or untested, and some can even be dangerous or cause bleeding, yes, even if they are natural (5). Here are my favorites – we often suggest Vitamin D, pharmaceutical grade fish oil (I buy mine from DrTheo.com) as well as Longvida brand curcumin 500 mg twice a day. Of course, these are not as powerful as anti-inflammatory medications and it may take time to see some benefits. Everyone should always clear every supplement and vitamin they take with their doctor and pharmacist beforehand as some supplements that are fine for one person may be dangerous for another. Some may interact with medications and cause serious problems, block medications from working or cause bleeding (6).
5. Medications– in addition to conservative therapies, it is wise to talk to the pain doctors about the option of a multi-week course of NSAIDs such as Aleve twice a day or once a day prescription meloxicam (Mobic) or celecoxib (Celebrex), all with uncommon but known risks for stomach and esophageal irritation or ulcer, kidney damage and other precautions. Some men take ibuprofen but we have found that it is very difficult for men to take ibuprofen (Advil) three times a day which is what is needed to achieve the anti-inflammatory benefits.
Prescription nerve pain meds such as Neurontin or Lyrica can help sometimes or even a several month trial of Testosterone Replacement Therapy (TRT) which works to suppress the production of sperm and fluid in the closed system so decrease the build up of fluid under pressure. In our experience, the testosterone therapy works in 1/3, does nothing in 1/3 and actually makes the pain worse in 1/3. Some antidepressants actually help to reduce pain. Narcotics are best avoided, do not solve the problem (they only mask the pain) and only make things much worse long-term with serious risks for addiction. Of course, all medications have the potential for risks and complications, some serious, even if tolerated before, so talk with all doctors to discuss the risks vs. benefits before starting any medication, and yes, even over-the-counter NSAIDs. Pharmacist are always a great resource as well.
Invasive treatments
6. Spermatic cord blocks, where the urologist injects numbing anesthetic medication (lidocaine and/or bupivicaine) into the tissues in and around the spermatic cord, high in the scrotum. The hope is that, if this works, this will block the delivery of the pain message from the nerves in and around the testicle up through the spermatic cord up to the brain. Though this may work for some, usually it only lasts a few hours to a day or so and has the added risks for causing more bleeding with more problems and pain to include damage to nerves or blood vessels. Cord blocks are controversial. Some doctors us this as a test and think that if this blocks the pain, then more definitive surgeries will help such as nerve stripping or neurolysis. Over the decades, I have seen many men that did not get a good cord block results yet had dramatically positive results with a vas reversal, so in my practice we do not routinely require or even perform a cord block before vasectomy reversal. I always worry that a cord block might cause more inflammation and scarring around the vas, making a subsequent vasectomy reversal surgery more challenging with concerns over lower success rates.
Destructive therapies
7. Nerve stripping, an outpatient surgery where the urologist would essentially peel the nerves off from alongside the vas and cord, again with the idea of preventing the message of pain from traveling up the nerves and getting up to the brain. I have seen and worry that this may or may not work and definitely creates tremendous scarring that can lower subsequent vasectomy reversal success.
8. Neurolysis, which is a newer treatment that is essentially a more advanced and focused version of the nerve stripping, where the nerves and nerve bundles inside the scrotum and groin that are the relay stations along the nerve paths are surgically removed, through a surgical microscope and often with the help of robotic assist (7). The hope is that this will also prevent transmission of the pain message to the brain, and for many men this can be effective, especially when performed by those few urologists who are experienced and skilled performing neurolysis procedures.
9. Partial or total removal of the epididymis, called an epididymectomy, where the urologist surgically removes all of part of the portion of the painful epididymis with the hope that the pain will go away. It does work for some men, but in my experience, more often than not, the pain persists and sometimes leads to more surgeries to remove more and more of the epididymis. A partial or total epididymectomy makes any future reverse vasectomy extremely challenging if not impossible.
10. Removal of the painful testicle (orchiectomy) can be effective for some, though I have seen some men with continued phantom pain even after the painful testicle is gone. I have never removed a testicle for pain but have seen many performed by other doctors, often as a first line treatment. Removing the testicle creates a number of questions. What do these other doctors recommend if there is pain in both testicles? What if the pain persists after the testicle is gone? How will surgical removal of one testicle impact on future testosterone levels as one gets older? Needless to say, I am not a fan of this treatment.
Reconstructive treatment
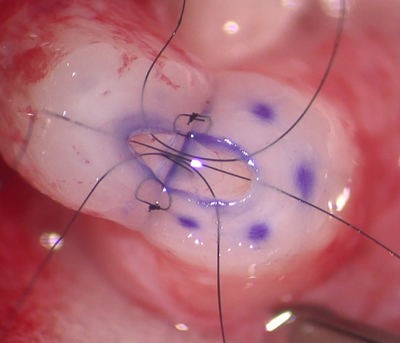
11. Vasectomy reversal, the only restorative treatment, where we remove under high power surgical magnification any and all scar from the vasectomy, sperm granulomas if present, the damaged, scarred vas, any metal clips or ties that remain. We then microsurgically reconnect the vas ends back together with a multi-layer (3 to 4 layers) microclosure to decompress the backed up fluid and restore the flow of sperm and fluid. This is a 2 to 2.5 hour outpatient surgery under mild sedation when done correctly by an true expert, with very high chances as high as 90 to 95% success with total resolution of the pain or such dramatic reduction that most men happily get on with their life (8). Most of our vas reversal patients have no pain afterwards and never even ask for a single Tylenol (acetaminophen).
It is important to know that in medicine, we all know that there are no guarantees how each person’s body will respond to any treatment. In general, when operating for pain, the three outcomes are – the patient will get better (the most common), he will stay the same or he could potentially get worse. Much of this will depend on the doctor, so choose wisely.
If there are any questions about how a vas reversal may be the right option, please call or contact us today to discuss the specifics of each person’s situation and answer any questions about vasectomy reversals and PVPS. Because we are not a pain management center, nor are we trained pain doctors, we cannot assume care or manage pain before or after the reversal. We are available to set up a phone call, office visit, Zoom, Skype or Face Time consultation (there is a charge) where the doctors can review how a state-of-the-art microsurgical vasectomy reversal at our full time, vas reversal only center may be the answer.
References:
1. Leslie TA, Illing RO, Cranston DW, et al. The incidence of chronic scrotal pain after vasectomy: a prospective audit. BJU Int 2007; 100:1330-3.
2. Sinha V, Ramasamy R. Post-vasectomy pain syndrome: diagnosis, management and treatment options. Transl Androl Urol. 2017 May; 6(Suppl 1): S44–S47.
3. Smith-Harrison LI, Smith RP. Vasectomy reversal for post-vasectomy pain syndrome. Transl Androl Urol. 2017 May; 6(Suppl 1): S10–S13.
4. Sinha V, Ramasamy R. Post-vasectomy pain syndrome: diagnosis, management and treatment options. Transl Androl Urol. 2017 May; 6(Suppl 1): S44–S47.
5. Mohan A, Lahiri A.Herbal medications and plastic surgery: a hidden danger. Aesthetic Plast Surg. 2014 Apr;38(2):479-81
6. Wong WW, Gabriel A, Maxwell GP, Gupta SC. Bleeding risks of herbal, homeopathic, and dietary supplements: a hidden nightmare for plastic surgeons? Aesthet Surg J. 2012 Mar;32(3):332-46.
7. Parekattil SJ, Cohen MS. Robotic microsurgery 2011: male infertility, chronic testicular pain, postvasectomy pain, sports hernia pain and phantom pain. Curr Opin Urol. 2011 Mar;21(2):121-6.
8. Smith-Harrison LI, Smith RP. Vasectomy reversal for post-vasectomy pain syndrome. Transl Androl Urol. 2017 May; 6(Suppl 1): S10–S13.
This page was reviewed, edited and updated January 8th, 2026 by Sheldon H. F. Marks, MD.